Introduction
In 2018, Lymphoma Coalition (LC) analysed data from the 2018 LC Global Patient Survey (GPS) on Lymphomas and CLL and determined that 'adequately informed' patients reported more positive healthcare experiences. From the 2018 survey, it was evident that many patients with lymphoma/CLL left their initial diagnosis meeting with a poor understanding of many aspects of their treatment and care plan. This can translate negatively across many areas of the patient experience.
LC used the 2020 GPS to further assess correlations relating to information provision and the patient experience. This study examines the relationship between the level of information patients with lymphoma/CLL received at diagnosis, and their level of participation in healthcare decisions and health management.
Methodology
This study is a sub-analysis of the 2020 LC GPS, which was available in 19 languages and was hosted online from 13 January 2020 until 13 March 2020. Globally, there were 11,878 respondents made up of 9,179 patients and 2,699 caregivers. This study includes patient data only.
Patients who felt they received the right amount of information at diagnosis (n=5159) were compared against patients who did not receive enough information (n=3285). Demographics of the two patient groups were examined, and questions relating to patient involvement in healthcare decision-making, disease management, and overall experience were analysed. Differences in proportions were tested using chi-square tests (p=0.05) and odds ratios with 95% CI. Statistical analyses were performed with IBM SPSS v21.
Results
The two patient groups (right amount of information 'RA', not enough information 'NE') were similar in their distribution of age and area of residence. The majority of patients in both groups were aged 50 years or older (71% RA; 60% NE) and lived in city/urban areas (47% RA; 55% NE). There were slightly more females than males in the NE group (61% female, 39% male) compared to the RA group (55% female, 45% male). Additionally, the majority of patients in the RA group lived in Europe (56%) while the majority of patients in the NE group lived in Asia-Pacific (44%).
Patients were asked if they are involved as much as they want to be in decisions about their care and treatment; the majority of patients in both groups said 'yes' (94% RA; 79% NE). However, only 4% of RA patients reported 'no, but I would like to be more involved', compared to 19% of NE patients.
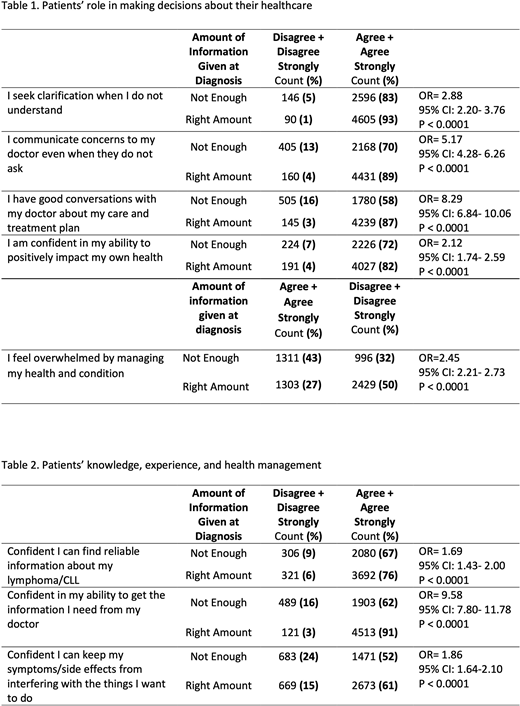
Patients were asked to indicate how much they agree or disagree with statements relating to their role in making decisions about their healthcare (see Table 1). Compared to RA patients, NE patients were at least twice as likely to disagree that they seek clarification when they do not understand (OR=2.88), that they are confident in communicating concerns to the doctor (OR=5.17), that they have good conversations with the doctor about their care and treatment plan (OR=8.29), and that they are confident in their ability to positively impact their health (OR=2.12). A greater proportion of RA patients reported agreeing with all of these statements. Further, compared to RA patients, NE patients were twice (OR=2.45) as likely to agree to feeling overwhelmed by managing their health and condition (Table 1).
Patients were asked questions relating to disease management and overall patient experience (Table 2). Compared to RA patients, NE patients were more likely to disagree that they are confident in their ability to find reliable information (OR=1.69), or in their ability to get the information they need from their doctor (OR=9.58). NE patients were also more likely to disagree that they are confident in their ability to keep their symptoms/side effects from interfering with the things they want to do (OR=1.86). A greater proportion of RA patients reported agreeing with all of these statements.
Conclusion
Compared to patients who felt they received the right amount of information at diagnosis, those who did not receive enough information were more likely to report disagreeing with all positive statements relating to involvement in healthcare decision-making, disease management, and overall experience. It was evident that patients who had knowledge surrounding their condition and care plan were more inclined to be confident in taking an active role in managing their health and condition. Access to credible timely information is therefore an important aspect to a successful patient experience.
Dren:Pfizer Inc: Research Funding; AbbVie Corporation: Research Funding; Takeda Oncology: Research Funding. Warwick:Pfizer Inc: Research Funding; AbbVie Corporation: Research Funding; Takeda Oncology: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal